Epidural Steroid Injections
What is the purpose of this procedure?
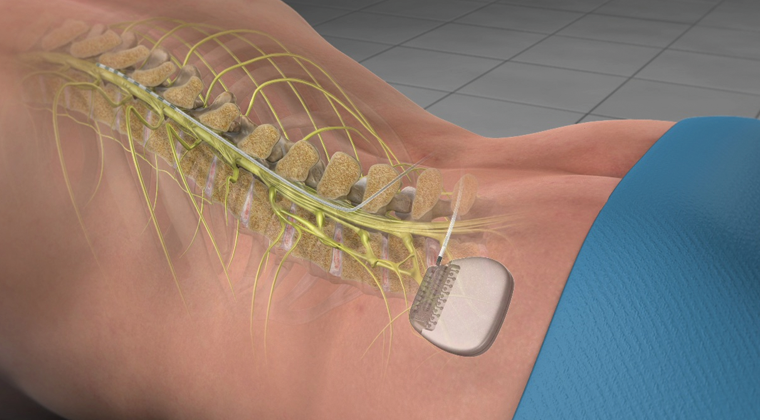
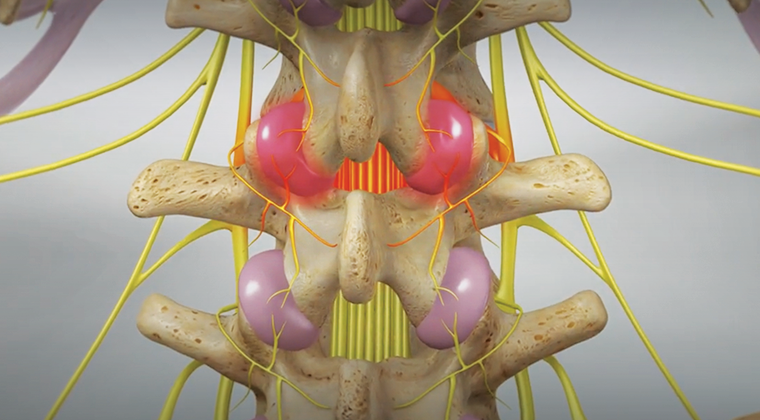
An epidural steroid injection places steroid into the epidural space of the spine to reduce inflammation (swelling) of spinal nerves and relieve back pain or sciatica. The injection may provide pain relief for a period of time while your body heals. It can also allow other treatments such as physical therapy to be more effective. (The epidural space is a canal-like space formed by the surrounding vertebrae that lie outside a sac that surrounds the spinal cord called the dura mater).
What are the risks associated with this procedure?
The risks for this procedure are infrequent. They include:
• Allergic reaction to medication
• Nerve damage (spinal cord and nerve roots)
• Bleeding and bruising at the injection site
• Pain at the injection site or during the injection
• Infection
• Puncture of the sac surrounding the spinal cord (dura mater)
• Injection of medication into a blood vessel or spinal fluid
• No improvement or worsening of your pain in some cases
• Steroid injections may cause a temporary increase in blood sugar, especially in diabetics.
How should I prepare for the procedure?
• You must have a driver with you at the time of check-in and check-out. Your driver must accompany you to the clinic for your procedure. You can be discharged only to the care of a responsible adult driver 18 years of age or older.
• It is important that you do not eat within 6 hours before the procedure. Small amounts of clear liquids are ok up to 2 hours before the procedure. If you are a diabetic, be sure to discuss an eating and medication schedule with your doctor.
• You may need to stop taking certain medications several days before the procedure. Please remind the doctor of all prescription and over-the-counter medications you take, including herbal and vitamin supplements. The doctor will tell you if and when you need to discontinue the medications.
• It is very important to tell the doctor if you have asthma or had an allergic reaction to the injected dye for a previous radiology exam (CT scan, angiogram, etc.). An allergic reaction has symptoms such as hives, itchiness, difficulty breathing, or any treatment which required hospital stay. The doctor may prescribe medications for you to take before having the procedure.
• Tell the doctor if you develop a cold, fever, or flu symptoms before your scheduled appointment, or if you have started taking antibiotics for an infection.
What will happen during the procedure?
The procedure is performed on an outpatient basis in a special procedure room equipped with a fluoroscope (x-ray).
- In the pre-procedure area, the nurse or doctor places an IV line. This is used for fluids and sedation.
- For your safety and comfort, when you get to the procedure room you will be connected to monitoring equipment (EKG monitor, blood pressure cuff, and blood oxygen monitoring device), and positioned on your stomach.
- Your back is cleansed with an antiseptic soap then the doctor injects numbing medicine into your skin. This will cause a burning sensation for a few seconds
- The doctor then carefully directs a needle with help of the fluoroscope (x-ray) to the epidural space. Contrast dye will be injected to help see the location better and ensure correct needle placement. The doctor then injects the steroid and anesthetic solution.
What should I expect after the procedure?
After the procedure you spend 20–30 minutes in the recovery area. Most people experience immediate benefit following the injection, but we encourage you to rest as much as possible the rest of the day. Avoid lifting heavy objects (groceries, children) along with physical exertion or straining. You may slowly resume your usual activities the following day. Some possible side effects include: reaction to medication (rare), bruising or pain at the injection site, flare-up of typical back pain, and temporary numbness or weakness.
Content supplied by:
Ronald Wasserman, M.D.
1.29.2020
Disclaimer: This document contains information and/or instructional materials developed by Michigan Medicine for the typical patient with your condition. It may include links to online content that was not created by Michigan Medicine and for which Michigan Medicine does not assume responsibility. It does not replace medical advice from your healthcare provider because your experience may differ from that of the typical patient. Talk to your healthcare provider if you have any questions about this document, your condition or your treatment plan. Patient Education by Michigan Medicine is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported (CC BY-NC-SA 3.0) License. Last Revised 06/2018.